 Shutterstock
ShutterstockThe COVID-19 pandemic is terrifying for many of us, but people with a disability have more reason to worry than most.
People with a disability often have underlying health conditions that make them more susceptible to serious illness or death if they contract COVID-19. They may also be more at risk of contracting the virus if they have disability workers entering their home.
The federal government has made several policy announcements to protect older Australians in aged care facilities, hospitals and GP clinics, but we’re yet to see the same consideration for people with disabilities.
Read more: Private hospitals get grace period before freeze on non-urgent elective surgery
People with disability are already disadvantaged
One in five people in Australia has a disability. Of these, more than three-quarters report a physical disability, although many report multiple types.
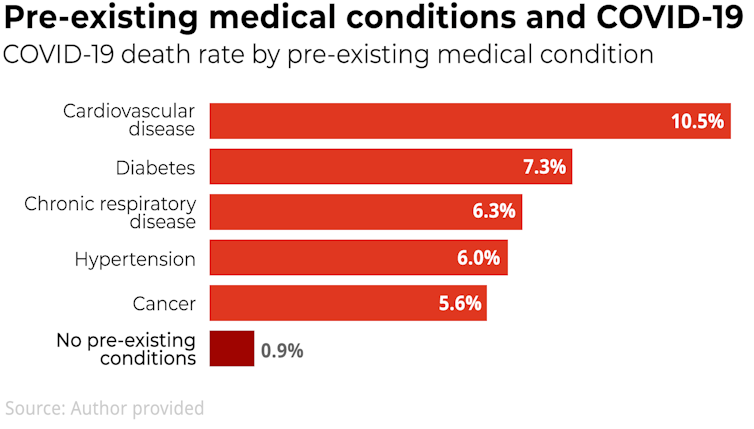
People with disabilities are at higher risk of serious illness and death from coronavirus death due to higher rates of co-exisiting health conditions such as diabetes, asthma and chronic pulmonary obstructive disease:
People with disability are more likely to be poorer, not working and more socially isolated. This makes them more vulnerable to poor health outcomes during the pandemic.
Evidence for previous pandemics shows that health inequities worsen during epidemics as more marginalised communities have fewer resources (financial and social) and struggle to access necessary supplies and services.
On top of this, health information is rarely presented in an accessible format for children and adults with intellectual disabilities, such as Easy English (a style of writing that’s simple and concise) and/or pictorial formats.
People with disabilities must not be de-prioritised
At a time when there is unprecedented demand for health services, we need to ensure people with disability don’t miss out.
Read more: How we'll avoid Australia's hospitals being crippled by coronavirus
Health services can be inadequate for people with disability at the best of times because of barriers such as physical inaccessibility, lack of understanding of a person’s disability, and cost.
We’ve already seen reports around the world that older people and those with disability have been de-prioritised in health services.
In Italy, the professional organisation that sets guidelines for intensive care has stated health resources should prioritise those with the highest chance of “therapeutic success”.
If people with disability have pre-existing health conditions, or if their particular impairment means their chance of recovery is diminished, they may be de-prioritised for intensive care.
Last week the Australia and New Zealand Intensive Care Society updated its guidelines for doctors, acknowledging that when the coronavirus pandemic peaks, difficult decisions may need to be made.
It recommends doctors make decisions based on the probable outcome, whether people have underlying health conditions, and the “burden of treatment” for the patient and their family.
The guidelines don’t mention people with disabilities, but it’s easy to see how an assessment of the “burden of treatment” could include people with intellectual disability becoming upset by treatment, or taking more time to deliver.
Access to protective equipment and support
For people who require support with activities of daily living (dressing, bathing, meal preparation, and so on) it’s likely they have one or possibly several care workers who will move in and out of their home every day.
Currently, many workers don’t have access to protective equipment, such as gloves and masks.
Disability care workers’ movement across multiple homes makes it likely that some of them will acquire and transmit COVID-19 to the people they care for.
Many of those working in care roles are among some of the lowest paid in our society and many are employed on a casual basis. If they don’t work a shift, they will not be paid.
This means we might be incentivising people who desperately need income to take risks with their health and the health of the people they’re supporting.
 Many people with disabilities don’t have the option of self-isolating.Shutterstock
Many people with disabilities don’t have the option of self-isolating.ShutterstockSome providers are choosing to cancel shifts and not put their staff at risk. This is one way to protect staff, but will leave some people with a disability in real need.
Even before this pandemic there were disability workforce shortages. This is likely to increase as the number of infections rises.
What should we do?
The following actions are urgently needed to protect people with a disability as the pandemic progresses:
the establishment of an expert committee with members who have expertise in the disability and health sectors to advise government
a new MBS item to develop COVID-19 health care plans with children and adults with complex disabilities, so they know how to implement social distancing and hygiene measures, and how to access tests and treatment
a dedicated coronavirus information hotline for people with disabilities, families and disability services, staffed by people with deep understanding of disability issues and underlying health issues
significant supplies of personal protective equipment (such as masks, gloves and gowns) for the disability support workforce to reduce transmission
government guarantees of income for care workers who may be sick, have caring responsibilities or have their shifts cancelled
the mobilisation of a broader disability workforce, for example by drawing on allied health students.
These actions won’t address all the inequities people with disabilities face, but they will be a good start.
Read more: Coronavirus will devastate Aboriginal communities if we don't act now
Helen Dickinson receives funding from the Australian Research Council The National Health and Medical Research Council and the Victorian and Commonwealth governments.
Anne Kavanagh receives funding from the Australian Research Council, the National Health and Medical Research Council and the Victorian and Commonwealth governments.
Authors: Helen Dickinson, Professor, Public Service Research, UNSW
| < Prev | Next > |
|---|







